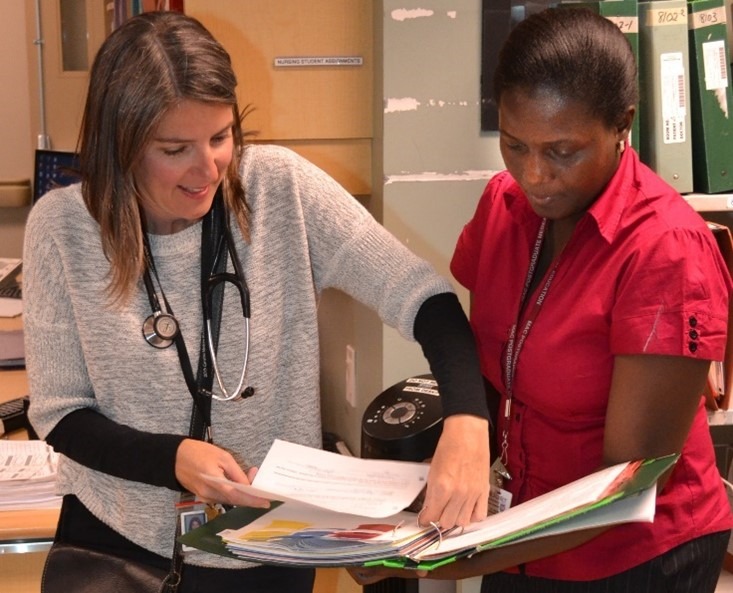
People in Hamilton may wonder why somebody would come all the way from Uganda to receive medical training here. What is life like in Uganda that would make you come all the way here for training? Dr. Nankabirwa: We do not have geriatric training at all in Uganda, in medical schools or in nursing schools. Even in all of Africa, there is no school that teaches geriatric medicine. We have our collaboration with the St. Joseph’s Health System International Outreach Program, and we have the staff and medical school residents of McMaster come to Uganda, specifically to Makerere University and Mulago National Referral Hospital, both in Kampala.
Why did you decide on geriatric medicine? Dr. Nankabira: I had a very loving grandmother, and I happened to stay with my grandmother during the holidays. My grandmother had a number of ailments, and each time she would get hospitalized, she would be treated but she would not heal very properly and then she would get back home not very fine. So I wondered why, what is really happening? So when I studied medicine, during my post-graduate training, I was like, “I was there, and I think that I would have done better, maybe.” I really chose geriatrics because I felt I should listen to these older patients, be kind to them. They needed somebody who really listens to them, is patient with them, someone who is able to shoulder them. I felt they needed to be loved and cared for in a different way. Then when I read a bit about geriatrics, I really saw that we’re not giving older patients the best treatment and care in Uganda, so that was another motive to specialize in geriatrics.
When did you come to the Hamilton? Dr. Nankabirwa: I came to Hamilton on 21st of September, 2015. I’m here for nine months. Originally I was here for six months. But I realized that we have a very different culture in terms of how we do the medicine, because we don’t really have the computerization, or the electronic data which is in Hamilton. So that takes time for me to learn, it also takes time for me to learn the culture of what happens, the common diseases that I should look out for. Yes, I come from an area where we have non-communicable diseases. But we also have lots of infectious diseases that may not be so common here. So that would take my time.
What have you learned here that you believe will really help you when you go back to Mulago Hospital and Makerere University?
Dr. Nankabirwa: One thing that I’ve really learned is the dementia, because at home we’re not really looking out for it, because we don’t really know so much about it. But now I think I really need to look out for it, because dementia is not just in the developed countries. It also affects the developing countries—that’s what I’ve learned.
I’ve also learned how to look out for delirium in patients, because we also do a lot of surgeries at home. We have so many people admitted who are having confusion, but the way it’s treated here is really very good. And at home I think I can use the same drugs that are in Hamilton.
The third thing that I’ve learned is elder abuse. I’ve seen the elder abuse and I think it can happen elsewhere. Because these are old people, they can be assaulted in any way, financially, physically. That’s another thing that I need to look out for. Because our people normally keep quiet, they’re suffering but they just keep quiet. And advocacy is important. I’ve seen there is lots of advocacy in Canada. So I think when I go back home I should do a lot of advocacy from within the hospital, within the Ministry of Health—everywhere that I can.
We are hoping that people who read this article about you and about the program will be inspired to help. How can they help?
Dr. Nankabirwa: Specifically, to my discipline of geriatrics, the population of older people in Uganda and Sub-Saharan Africa is actually growing. And we don’t have any geriatricians in Uganda. So, we need people to specifically take care of the ailments of older patients. And their ailments present in a different way. And they have their own ailments that affect them as an age group.
So, we really need to support them. We need more doctors. We need to try to change the attitude of the young people, the young doctors and even the senior doctors to really embrace all these changes. People can help support the training of more doctors, because when I go back home, I’m not going to be running from clinic to clinic, clinic to clinic. I feel I’m going to do more capacity building. And if I do more capacity building, that means there is too much work for me as one person.
If we trained more people, maybe five or ten more doctors, I think that would be very good. Some will be able to do capacity building, others will be able to treat the patients, to do clinical work basically, others to advocate.
What’s your experience been like here at St. Joes as a hospital?
Dr. Nankabirwa: It’s been a very good experience. I’ve been supervised, so my confidence has improved. I see patients on my own, and then discuss them with my supervisor. And tell her about my decisions, what I feel for the patient, and we write it down and see this person walk home alive, which makes my heart very pleased that I can also make a decision in Canada for the Canadian population and they get better. So, it’s been a good experience, and I have a good relationship with the patients.
I’m happy that I’m even allowed to touch patients, because I know some universities and hospitals don’t allow doctors from elsewhere, not trained from their countries, to touch patients. I’ve seen colleagues leave Uganda go very many miles and only to go to observe.
Have you got anything else that you would like to add, any final thoughts?
Dr. Nankabirwa: I want to say thank you to my program director and all the staff. It was a very good privilege to come and be accepted—accepted in the system. I’m also very thankful to the International Outreach Program, thankful to all the hospitals, including St. Joes and Hamilton Health Sciences, for accepting me to train. I believe I’m going to make a good geriatrician.
Dr. St. Onge, what’s the experience for life for you with Harriet being here?
Dr. St. Onge: This was a bonus for our division. Whenever you work with someone who has a different outlook and experience, it certainly enriches your own work environment. It’s great for her to have a variety of exposure at the different hospitals, and it’s been great for everyone in our division who has had a chance to work with her.